Improving management consultancy use in the NHS
Translating research into practice following findings of inefficient use of external management consultants.

Consultancy controversy
Use of external management consultants in the public sector is growing, with the sector spending around £2.8bn in the UK in 2022. Organisations use consultants to help with strategic advice, organisation and financial planning and change implementation. Their explicit aims are typically to help improve organisational performance, boost efficiency and achieve cost savings. They are not always effective but are always controversial.
Andrew Sturdy, Professor of Management and Organisation at the University of Bristol Business School, believes the roles of management consultants can be summed up by the acronym FEEL – ‘Facilitators, experts, extras and legitimators. The final role is controversial – if you or I were to recommend something, it wouldn't have the same clout as a consultant you are paying large amounts of money for.'
As Professor Sturdy notes, controversy can stem from the risk that consultants are being used to push through and ‘legitimise’ decisions a client organisation has already made, but also from being less efficient or effective than other approaches. Thus, critics also claim that organisations have developed an over-reliance on, or even addiction to, use of external consultants for management advice.
The NHS is a prime example of a public sector organisation using external management consultants, with trusts in England each spending an average of £1.2 million on external consultancy fees per year[1], and some spending up to £5.6 million. With the current financial pressures the NHS is faced with, this poses the question, are management consultants key facilitators of improvements to our healthcare system, a waste of precious NHS funding or in need of much more effective governance?
[1] Average spend per year from a sample of 120 NHS trusts studied between 2008 and 2013 - ‘The impact of management consultants on public service efficiency’| 2019 study.
The verdict
With limited transparency around the use of consultancy in the NHS and its effects, research by academics at the Universities of Bristol, York and Seville over the last 5 years has aimed to explore just such a question. The team looked at the effectiveness and governance of management consultancy use in the NHS and examined data from over 120 NHS trusts. Their findings evidenced that, rather than creating efficiencies, greater spending on external management consultants by NHS trusts often led to increased inefficiency in those trusts, while inflating further demand for external consultants.
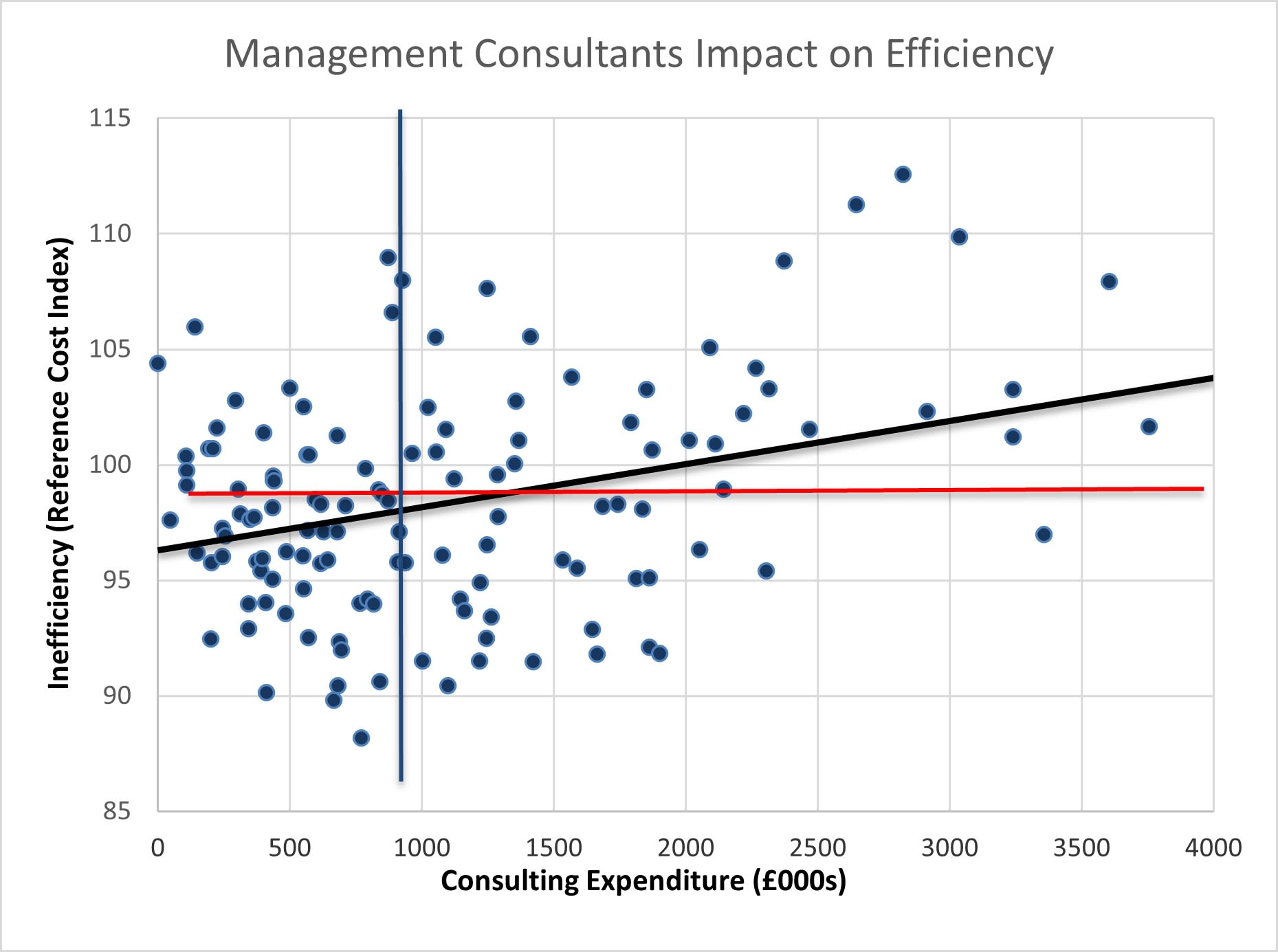
Scattergraph key: Blue line - median consulting expenditure, Red line - median level of efficiency (Reference Cost Index), Black line - trendline, showing that higher consulting expenditure is associated with greater inefficiency (or higher costs).
Scattergraph key: Blue line - median consulting expenditure, Red line - median level of efficiency (Reference Cost Index), Black line - trendline, showing that higher consulting expenditure is associated with greater inefficiency (or higher costs).
Issues of inefficiency
This inefficiency was measurable and stark. Greater use of external management consultants was shown to reduce efficiency in the trusts by 3.5% to 8%, depending on the standard measure used, and while a small number of trusts did see slight efficiency improvements, the resounding overall effect was negative.
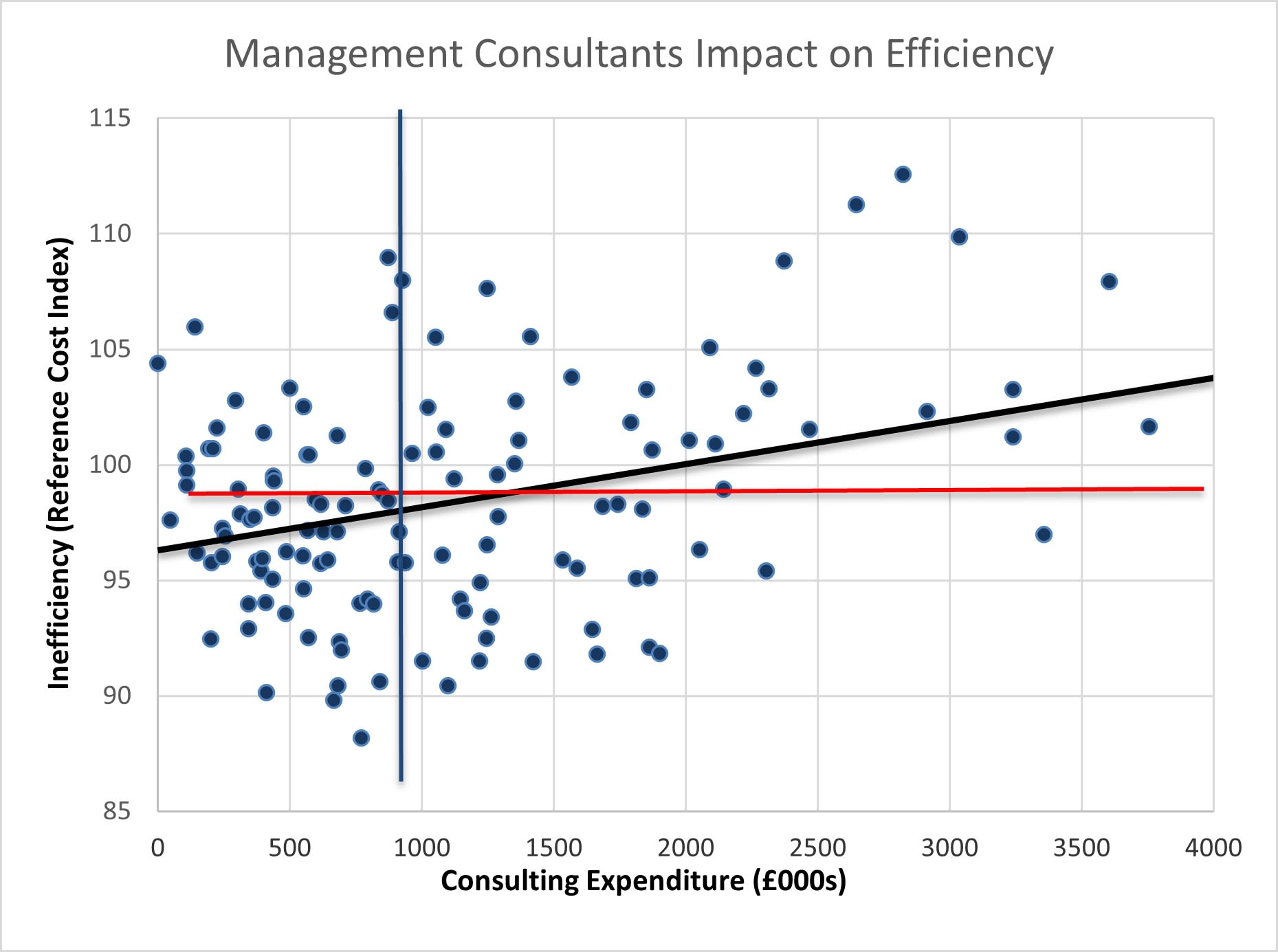
Scattergraph key: Blue line - median consulting expenditure, Red line - median level of efficiency (Reference Cost Index), Black line - trendline, showing that higher consulting expenditure is associated with greater inefficiency (or higher costs).
Could it be that already inefficient trusts happen to be using management consultants more? Data analysis by the researchers suggests this is not the case and points instead to the conclusion that it is the increased use of external consultants itself that is associated with this increase in inefficiency.
These findings suggest financially that management consultants are not currently saving the NHS money and are instead costing them. Professor Sturdy observed, ‘In financial terms, the average annual losses of hospitals that used management consultants were quite small: £10,600 for each hospital trust. But this does not take into account the management consulting fees paid, which amounted to £1.2m per trust per year on average. This roughly equates to the salaries of 20 managers, ten consultant doctors or 35 senior nurses for each trust.’
Practically, findings also highlighted that patient outcomes were not seen to have been improved by greater use of management consultants, with evaluation of patient experience scores showing that external consultant use had no significant impact on the quality of hospital services.
Tackling overuse
Despite a lack of improvement to efficiency, demand inflation was found where higher use led to continued hiring of consultancy. This suggests the likelihood of ‘over-use’ of management consultants within the NHS.
In fact, surprisingly, external consultants did not seem to be a means used to cover in-house management shortages or ‘hollowing out’ - trusts with more managers were actually those using external consultants the most. This was less the case where there were higher levels of internal consultants which implies that building internal specialist capability could reduce spending on external consultants. Adding further merit to this theory, emerging research findings suggest that internal specialist NHS managers may perform better overall than external consultants, producing mostly more efficient results.
Reducing this over-use of external consultancy and comparing outcomes of using interval versus external consultants are key focuses of the researchers going forward, with Professor Sturdy highlighting, 'Our research raises serious questions about the use of external consultancy, but this is not the issue. The problem is their 'over-use' and everyone would agree that this needs to be urgently addressed.'


Troubles with transparency
Prior to the team’s research, there was a lack of clarity around the outcomes and efficiencies of using external consultants. Previous data has mostly been provided directly from consultants and clients themselves, and this has resulted historically in biased results that are hard to draw reliable conclusions from. Even now, consultants and clients are both sometimes motivated to protect their reputations and as a result, failed projects can sometimes be buried to prevent negative perceptions and yet consultants are typically rewarded regardless of performance with fees still being paid.
This research aimed to overcome that, using publicly available measures of efficiency and previously inaccessible information on spending on consulting within NHS trusts, to provide greater transparency and a less subjective or partial view.
From a range of different studies conducted, including at national and local levels, the research has raised serious questions about accountability, performance and, ultimately, value for money. It suggests that existing approaches to governing external consultants are insufficient and/or have not been fully adopted. These therefore need to be strengthened and alternatives should be sought and implemented. This is now the focus for the team.

Impact and policy implications
With funding from Research England (QR Policy Support Fund), Professor Sturdy and colleagues will work with both the NHS and consultancy partners and leverage their findings to translate research into practice. Working with partners, they will help to improve the use of NHS resources through development of new practices, sharing knowledge and exploring alternatives to using external management consultants.
The project will run until July 2024 and their continuing research will also reveal the efficiency of internal verses external specialists to help inform practice, either by improving use of external consultants or developing internal resources.
This research and the impact project associated with it have the potential to create significant financial savings for the NHS, freeing up funding for them to spend in other areas. Such savings would have very real and practical implications for the NHS as Professor Sturdy summarises, ‘If we can help effect savings within the NHS, that's going to affect their healthcare delivery directly’.



